Regenerative Therapy Has Potential to Treat Chronic Joint Dislocation
Regenerative treatment with tetradecyl sulfate and polidocanol injections helps stabilize joints in Ehlers-Danlos syndrome (EDS) patients with recurrent joint dislocation, a reassessment of medical records shows.
The study, “Comparison of tetradecyl sulfate versus polidocanol injections for stabilization of joints that regularly dislocate in an Ehlers-Danlos population” was published in the journal BMJ Open Sport & Exercise Medicine.
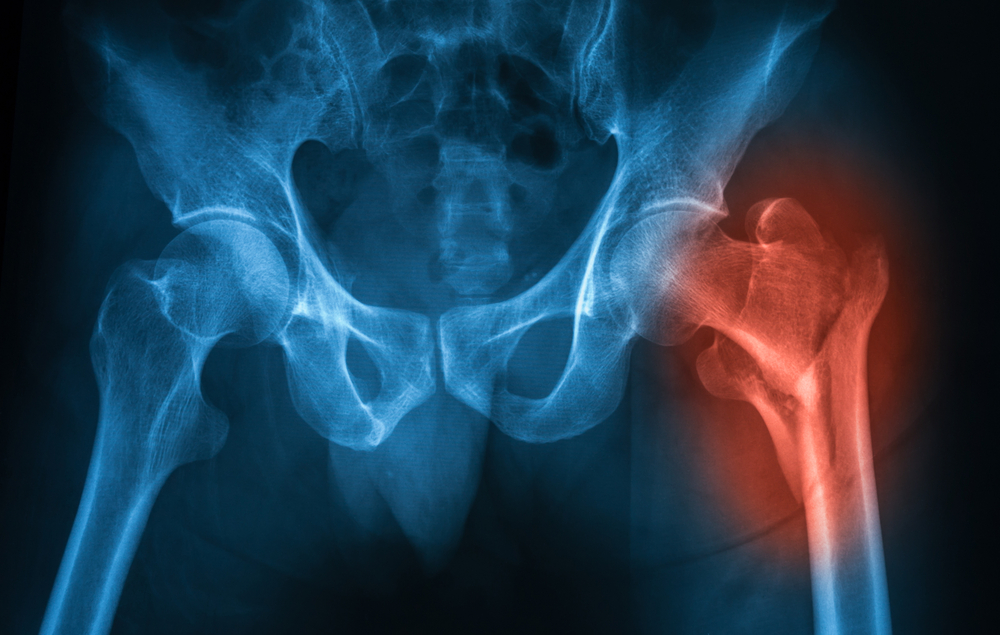
EDS is a genetic condition that affects the connective tissues that support the bones, skin, and other organs. Defects in connective tissue can result in loose joints, causing frequent dislocation, a symptom noted in about one-third of EDS patients.
Prolotherapy or sclerosant therapy is a type of regenerative treatment in which a medication that promotes tissue regrowth is injected at the site of damage. This can promote joint strengthening and prevent further damage.
Sclerosant therapy has been used for a long time to treat other conditions such as varicose veins, hemorrhoids, and knee ligament injuries. But their use in treating EDS joint dislocations has not been well-studied.
Now, Fraser Burling, a physician and rheumatologist at the Rheumatology and Musculoskeletal Clinic, Remuera, in New Zealand, analyzed medical data from EDS patients with a history of joint dislocation who had been treated with one of the two sclerosant agents: tetradecyl sulfate and polidocanol.
Medical records of 46 patients (ages 18–75) who were treated at a single center in New Zealand were analyzed. In these patients, joint dislocation was mostly in the shoulders, hips, knees, and ankles.
Records indicated that the patients received either 0.11% tetradecyl sulfate solution (37 patients) or 0.25% polidocanol solution (nine patients) injections in the connective tissue near the site of joint dislocation. There was a mean interval of four weeks between injections if the same area required more medication.
The medication was administered only after the bones were returned to their normal position by trained specialists, and the treatment was considered successful if the dislocated joint was stabilized and did not loosen again at the three-month follow-up visit after the last injection.
Data for a three-year follow-up period were evaluated. The tetradecyl sulfate group cumulatively received 305 injections around 97 joints; the polidocanol group had a total of 36 injections around 19 joints.
Results showed that both groups reported successful treatment. No further dislocations in the treated joints at the time of follow-up were reported, and there was no statistically significant difference between the therapies.
Regarding adverse events, the injections were painful, and some caused a bruise that lasted about three to five days. No other significant side effects were reported.
After the treatment, “the level of pain reduced, and the patient ended up with little or no pain in the joints treated. Quality of life improved as well,” researchers stated.
Overall, “there was no difference between the two groups for stabilizing joints from dislocating. These two agents appear promising for treating patients with recurrent joint dislocations in the setting of EDS,” the researchers concluded.
Multi-center, randomized, controlled trials are, however, needed to confirm these data, the team noted.