EDS Patients Have Increased Blood Artery Stiffness, Linked to Cardiovascular Disease Risk
Written by |
People with Ehlers-Danlos syndrome (EDS) have significantly greater stiffness of their blood arteries — a known risk factor for cardiovascular disease — than their healthy peers, a Swiss study shows.
While vascular EDS (vEDS) was associated with the highest arterial stiffness among the different EDS types, these differences did not reach statistical significance.
Further studies are needed to assess the predictive value of increased arterial stiffness in terms of general cardiovascular risk in EDS patients, the investigators noted. Additional research also is warranted for aortic disease progression — as reported for people with Marfan syndrome, another connective tissue disease — they said.
The study, “Increased augmentation index in patients with Ehlers-Danlos syndrome,” was published in the journal BMC Cardiovascular Disorders.
EDS comprises a group of genetic disorders that affect the connective tissue — the tissue that provides support to structures such as joints, blood vessels, and skin. These disorders generally are characterized by tissue fragility, joint and skin hypermobility, and blood vessel fragility. Of note, hypermobility means that patients’ joints or skin extend or stretch beyond normal.
While aneurysms and rupture of medium to large arteries are hallmarks of vEDS, the most lethal form of the disease, increased bleeding tendencies and major vascular events have been reported in people with non-vascular types of EDS.
However, “reliable prognostic factors predicting vascular disease progression (e.g. arterial aneurysms, dissections, and ruptures) in EDS patients are still missing,” the researchers wrote.
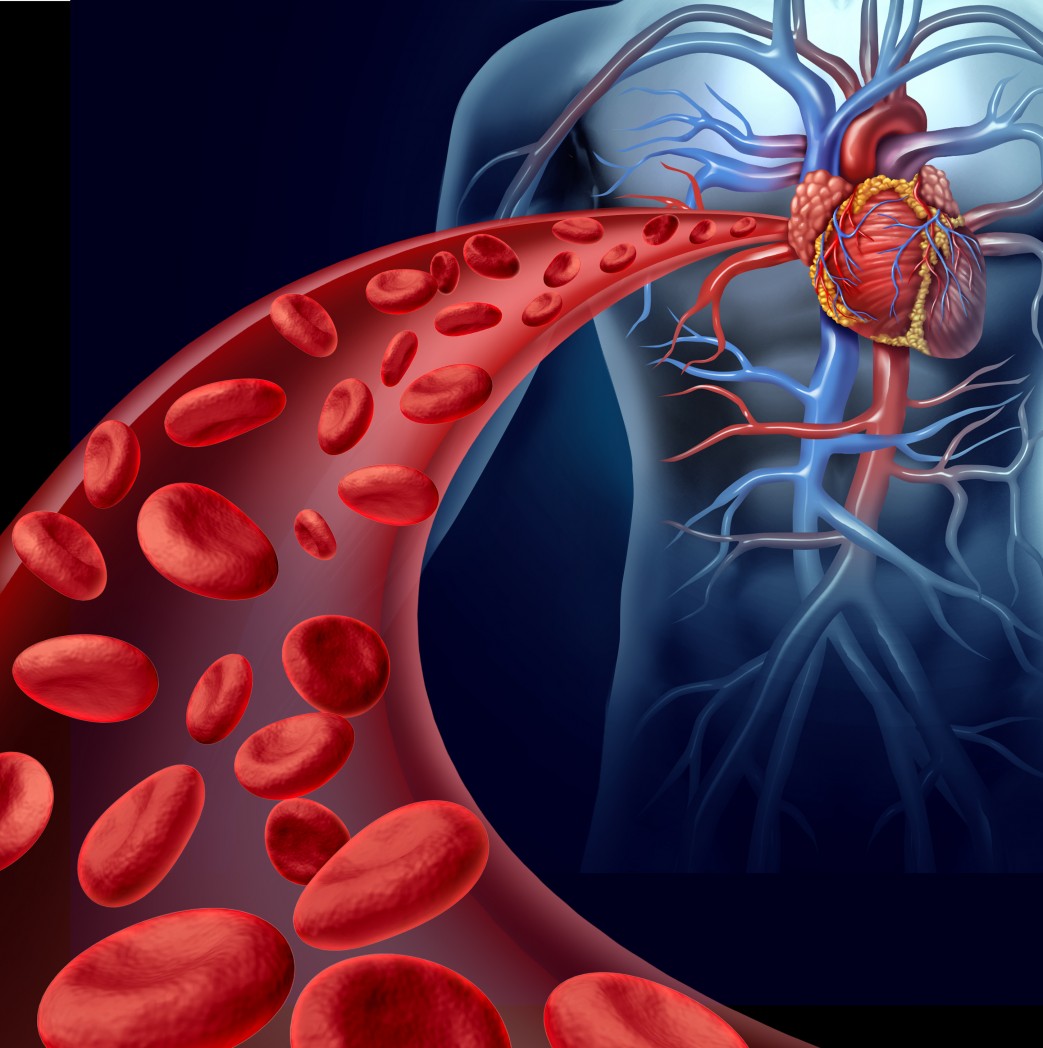
Previous studies have shown that the augmentation index (AIx), an indirect measure of arterial stiffness and a marker of cardiovascular risk, was increased and associated with aortic disease progression in people with Marfan syndrome. These patients also suffer from fatal vascular events.
Now, researchers in Switzerland set out to evaluate whether AIx-based arterial stiffness was elevated in EDS patients, and to identify potential predicting factors for arterial stiffness.
AIx-derived arterial stiffness was assessed in 61 adults with EDS — 43 women and 18 men with a mean age of 39.3 years — and 61 age-, gender-, height-, and weight-matched healthy individuals. The investigators used a non-invasive testing method called arterial applanation tonometry.
The patients had been living with an EDS diagnosis for a mean of 10 years. The disease in 11 participants (18%) remained unassignable due to overlapping features. Among the rest, 26 (43%) had hypermobile EDS, 21 (34%) had classical EDS, and three (5%) had vEDS.
Of note, blood pressure and the use of blood pressure medications and nonsteroidal anti-inflammatory drugs were significantly higher among EDS patients than in healthy people.
The results showed that EDS patients had significantly increased AIx (22.8% AIx), compared with their healthy peers (14.8%), who showed levels within reference values obtained from larger studies. The participants with vEDS showed the highest AIx, but differences between the groups did not reach statistical significance, likely due to the small patient number of EDS subtypes, especially of vEDS, the researchers noted.
Further analysis highlighted that having EDS was a significant and independent predictor of high AIx. So too was being a woman, being older, having a smaller stature, having higher blood pressure, and smoking more, all factors that were consistent with previous studies. Notably, medication use was not independently associated with AIx.
These findings suggested that the presence of higher arterial stiffness in all EDS patient types, independent of known influencing factors, highlight a potential “increased risk for cardiovascular events beside the vEDS-typical vascular complications,” the researchers wrote.
“Since vEDS patients harbor the highest risk for fatal vascular events and this subgroup presented the highest AIx in our study, AIx already indicate potential as a possible predictor for vascular high-risk patients,” they added.
While there is limited data on arterial stiffness in people with EDS, these findings contradict a previous study showing increased arterial elasticity in this patient population. These differences may be associated with distinct patient populations and measures of arterial stiffness, the researchers noted.
Further research, using several arterial stiffness measuring methods, is needed to confirm these findings. Future studies also are needed to assess the general cardiovascular risk in EDS patients, compared with the general population, as well as the predictive value of increased arterial stiffness for cardiovascular outcomes, including aortic disease progression as shown for Marfan syndrome.