Abnormal Blood Vessel Communication May Support Early Diagnosis of Vascular EDS, Researchers Suggest
Written by |
A type of abnormal communication between the main blood vessels in the head, called carotid-cavernous fistula, may be the first manifestation of vascular Ehlers-Danlos syndrome (vEDS) among seemingly healthy young individuals, researchers reported in a recent study.
The study, “Pathophysiology of carotid-cavernous fistulas in vascular Ehlers-Danlos syndrome: a retrospective cohort and comprehensive review,” was published in the Orphanet Journal of Rare Diseases.
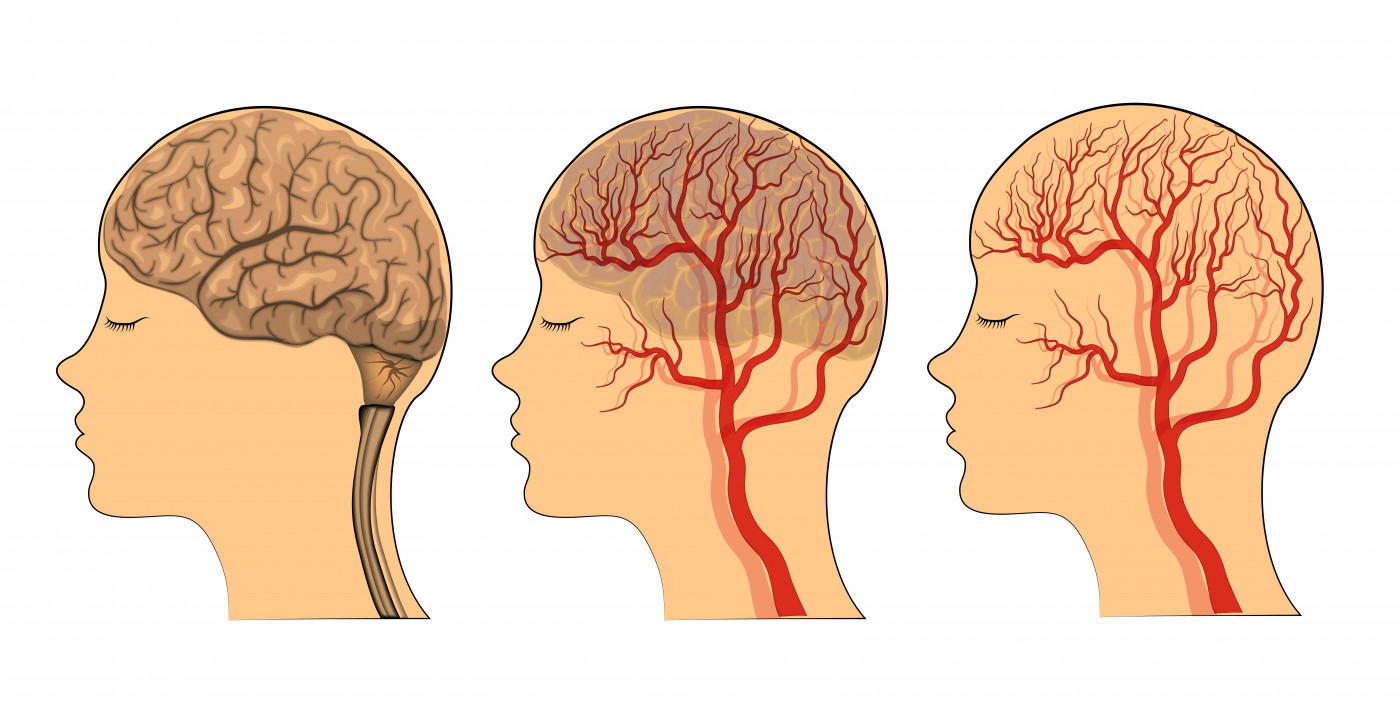
Carotid-cavernous fistula (CCF) is an abnormal communication between the arterial and venous systems in the head, which carry oxygenated and non-oxygenated blood, respectively.
In direct CCF, the carotid artery wall disrupts oxygenated blood from entering the venous system, causing a short-circuiting of the blood flow. This event is often detected by the swelling of the eye, pain, paralysis of the muscles surrounding the eye, and vision loss.
In the general population, direct CCF is a rare event and usually does not occur spontaneously but rather due to trauma, surgery, or the rupturing of an aneurysm. However, it is commonly found in patients with vEDS, mostly due to the fragility of the vessels’ wall caused by the lack of type III collagen, which is characteristic of the disease.
To further evaluate the incidence and characteristics of spontaneous direct CCF in this population, a research team reviewed the clinical records of 133 patients with confirmed vEDS.
Among these patients, 13 had suffered a spontaneous direct CCF, of whom 12 were women. A review of available literature revealed that 79.4 percent of reported vEDS patients who experienced direct CCF were women.
This increased incidence may be partly explained by the anatomical differences of blood vessels between men and women, but also hormonal differences, the researchers noted.
Analysis of the genetic variant of the COL3A1 gene carried by these patients — the underlying genetic cause of vEDS — revealed that the patients had two specific types of mutations: Glycine missense substitutions and splice-site variants.
This finding suggests that patients with these types of genetic abnormalities may have an increased risk of experiencing direct spontaneous CCF.
In nine patients in the cohort analyzed, direct CCF was the first symptomatic vascular complication. Interestingly, this event occurred even before vEDS had been diagnosed in eight of these patients, and it only prompted further investigation for vEDS in four cases.
“As direct spontaneous CCF in young patients seems to be [a high-risk feature] of vEDS, … type III collagen deficiency should be suspected” and “genetic testing of the COL3A1 gene should be mandatory,” the researchers wrote.
Also, the team believes that spontaneous direct CCF is linked to the type of COL3A1 variant, with Glycine missense substitutions and splice-site variants being associated with a higher risk.