Periodontal EDS Linked to Changes in Brain’s White Matter, Case Series Finds
Written by |
Patients diagnosed with periodontal Ehlers-Danlos syndrome (EDS) may also have changes in the brain’s white matter, which makes up the tissue in the brain and spinal cord, a case series reports.
Periodontal EDS is the rarest form of EDS, and is characterized by severe early-onset gum disease.
The study, “Peridontal Ehlers-Danlos syndrome is associated with leukoencephalopathy,” was published in the journal Neurogenetics.
Periodontal EDS is caused by mutations in the C1R or C1S genes, which are part of the classical complement pathway, known to regulate microbial-host interactions, including inflammation.
Clinical presentation of periodontal EDS is characterized by a premature loss of teeth due to severe gum inflammation, and increased frequency of infections. The condition is also associated with other connective tissue problems, such as easy bruising, leg skin discoloration, joint hypermobility, and organ/vessel ruptures.
Although EDS is not commonly correlated with neurological symptoms, some cases of neurological abnormalities in these patients have been reported. In periodontal EDS patients, up to now, there was only a single case report of leukoencephalopathy, a condition that affects the brain’s white matter.
Now, a team of researchers in Austria and the Netherlands are reporting a series of cases of patients clinically and genetically diagnosed with periodontal EDS who also had leukoencephalopathy.
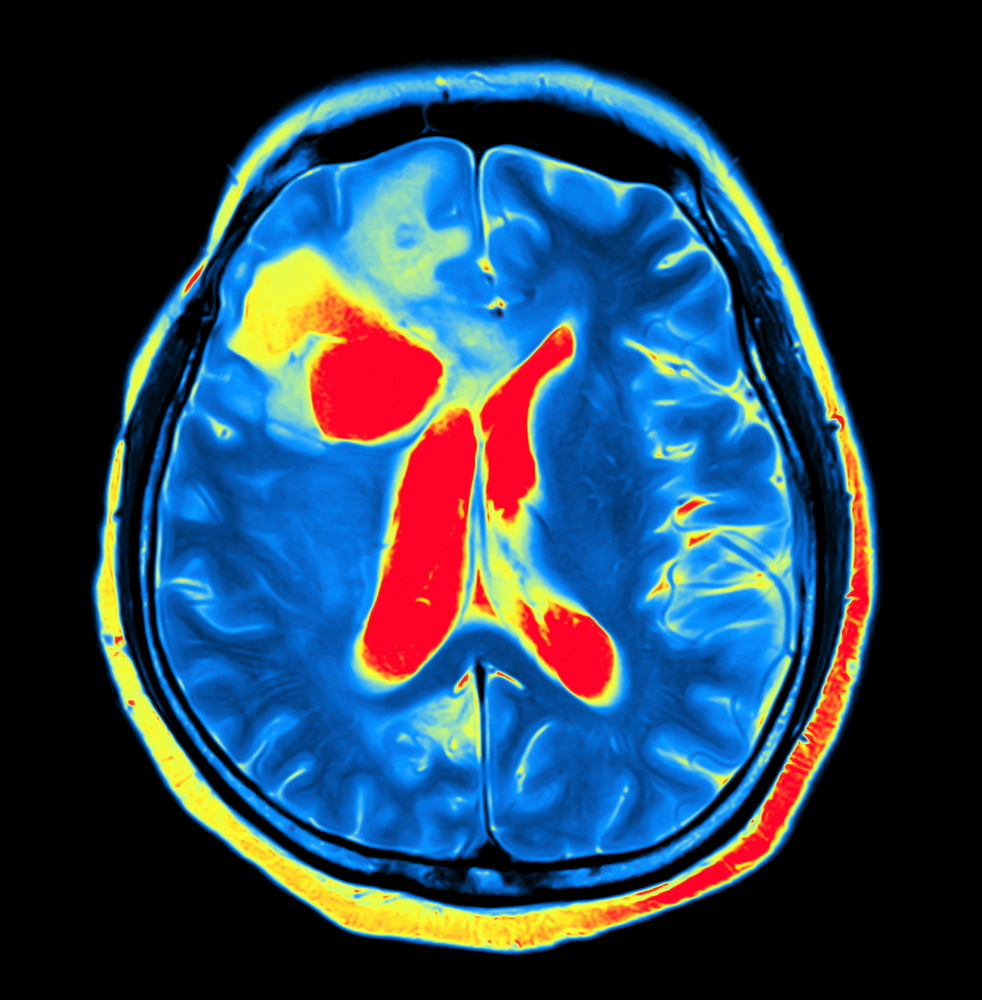
A total of eight individuals, seven adults and one child, belonging to two Caucasian families (a Dutch and an Austrian family), previously diagnosed with periodontal EDS, were evaluated by general physical exams, genetic analysis, and neurologically through magnetic resonance imaging (MRI).
The genetic analysis showed that all patients had a mutation in one of the two copies of the C1R gene.
Brain MRI images showed that the only child (8 years old) enrolled had a normal brain scan result, while all seven adult patients had brain white matter abnormalities.
Specifically, the young adults showed some changes in deep brain cerebral white matter and enlarged perivascular spaces (interstitial fluid-filled spaces in the brain) on MRI scans. In older patients, leukoencephalopathy was evident, as well as tissue lesions in the brain. Nonetheless, only one of the patients showed clinical neurological symptoms, namely a mild cognitive decline.
According to the team, the MRI pattern found in adult periodontal EDS patients’ brain white matter suggested alterations in small blood vessels that are consistent with small vessel disease.
A biopsy performed on one of the patients revealed small vessel vasculitis, which causes the fragility of capillaries (small blood vessels). However, the team was unable to confirm if this vascular condition was the underlying cause for the lesions observed in the white matter of the patient’s brain.
The team concluded that “in both families, periodontal EDS is associated with an adult-onset leukoencephalopathy,” and that “leukoencephalopathy appears to be part of the clinical spectrum in periodontal EDS with C1R mutations.”
Based on the results, the researchers suggested a possible link “between the classical complement pathway, connective tissue, brain small vessels, and brain white matter abnormalities,” although further studies are needed in patients with periodontal EDS to clarify the exact cause of the disease and potential neurological consequences.


