Vascular EDS Appears as Fast-growing Neck Mass in UCSF Case Study
A case of vascular Ehlers-Danlos syndrome (vEDS) which appeared as a rapidly growing neck mass was reported by researchers at the University of California San Francisco (UCSF) Medical Center.
The case was described in the study, “Vascular Ehlers-Danlos Syndrome Presenting as a Pulsatile Neck Mass: a Case Report and Review of Literature,” published in the Journal of General Internal Medicine.
The patient, a 30-year-old woman, was admitted to the hospital due to a painful neck mass on the right side that had been rapidly growing over three weeks.
She had been previously diagnosed with an inflammation of a parotid gland (parotitis) in another hospital, for which she underwent a two-week treatment with the antibiotic cephalexin. But the treatment had no apparent effect and the neck mass continued to grow.
The woman had a history of varicose veins in her legs, although she had received treatment to correct it. Her family had no history of bleeding predisposition or of connective tissue diseases. She said she had not suffered any trauma or injury to her neck, face, or jaw that could explain the growing mass.
A physical examination revealed a mass measuring 3 centimeters on the right side of her neck with surrounding tissue swelling (edema). She also had a violet-color net-looking rash overlying the neck mass region.
Her skin did not show increased elasticity, although she had increased mobility of the joints, especially in the fingers and shoulders.
“In patients with these features, vascular Ehlers-Danlos syndrome should be suspected and genetic testing should be completed to confirm the diagnosis,” the researchers wrote.
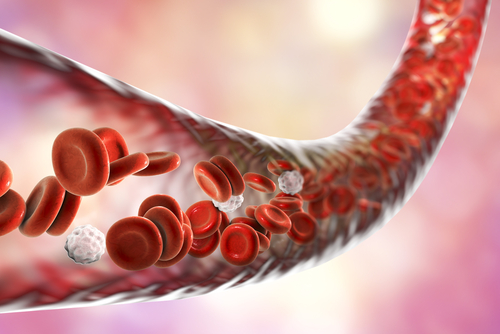
Vascular Ehlers-Danlos syndrome mainly affects blood vessels, and it often appears as vascular aneurysms and vessel rupture, leading to hemorrhages.
Blood analyses were all negative for infections, inflammation, or autoimmune antibodies. Also, the patient did not have any symptoms of cardiovascular, pulmonary, abdominal, or neurological problems.
It was possible to detect the blood flow rhythmic pulse in the neck mass (pulsatile mass), suggesting that it could be due to an aneurism — a bubble-like overgrowth of a weakened blood vessel.
Analysis of the neck by computer tomography angiography (CTA) scan confirmed the patient had an aneurism measuring 2.7 cm arising from the maxillary artery and another one measuring 4 mm in the carotid artery.
A CTA scan of the brain revealed she also had a 3 mm aneurysm in the left middle cerebral artery.
Given the broad range of manifestations, the attending physician consulted specialists at the rheumatology, otolaryngology, interventional radiology, and vascular surgery departments.
After multidisciplinary discussions, they believed the patient’s condition was consistent with a diagnosis of vascular EDS.
Genetic testing revealed a COL3A1 gene mutation, which confirmed the suspected vascular Ehlers-Danlos diagnosis. Genetic counseling was provided to inform the patient and her family of the risk of inheritance and pregnancy.
“As described in this case, management of a suspected connective tissue disorder is a multidisciplinary approach including vascular surgery, medical therapy, and genetic testing to confirm the diagnosis,” the researchers wrote.
The patient underwent vascular surgery to address the neck mass, which was performed without complications. She recovered completely from the surgery and was discharged. She started treatment with carvedilol to prevent the rupture of arteries, and oral contraception to prevent pregnancy due to the risk of uterine rupture.
The difficulty of detecting blood vessel abnormalities in physical examinations in patients with vascular EDS often delays the diagnosis until the patient has life-threatening complications, the team wrote.
Vascular EDS has a relatively poor prognosis due to the increased fragility of blood vessels, which can lead to internal bleeding. Given this, prompt diagnosis and close monitoring are crucial to increase patients’ survival.