COL3A1 Mutations Linked to Altered Structural Proteins in Vascular EDS, Study Finds
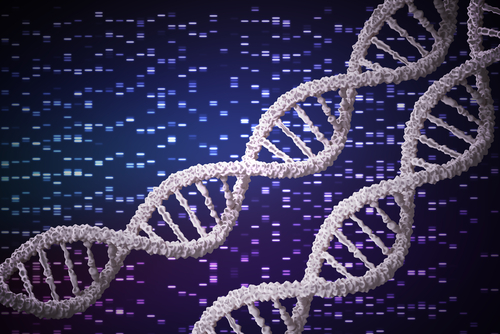
Mutations in the gene COL3A1, responsible for the development of vascular Ehlers-Danlos syndrome (vEDS), are associated with alterations in several structural proteins, according to researchers.
The study, “Transcriptome analysis of skin fibroblasts with dominant negative COL3A1 mutations provides molecular insights into the etiopathology of vascular Ehlers-Danlos syndrome,” was published in the journal PLOS One.
The vascular type of Ehlers-Danlos syndrome, the most serious form of EDS, is caused by a mutation in the COL3A1 gene. This gene provides information to produce a protein called type III collagen (COLLIII), which is the predominant collagen protein present in blood vessels and hollow organs.
Collagen is one of the main structural proteins of the extracellular matrix (ECM), which provides structural and biochemical support to cells.
A lack of COLLIII leads to increased bruising, arterial and bowel rupture, tendon and muscle rupture, and uterine, cervical, and vaginal fragility during pregnancy and delivery.
In the study, researchers used skin cells from three patients with vEDS with different COL3A1 mutations and performed a transcriptome-wide expression profiling — a common method to determine gene expression patterns (the genes that are activated or repressed).
Results from the analysis showed there were significant changes in the levels of genes involved in ECM organization, endoplasmic reticulum (ER) stability, folding of collagen proteins, formation of proteasomes (protein degradation machinery), and cell cycle regulation.
Earlier studies have shown that not only is COLLIII abnormally produced in vEDS, but its deposition in the ECM is also affected.
Researchers investigated whether a deficiency in COLLIII protein led to abnormal levels or deposition of other structural proteins.
They discovered that impaired expression of COLLIII was associated with a disassembly of fibrillins, EMILINs, and elastin — all important components of the ECM.
The team also found that the levels of the ER protein disulfide isomerase (PDI) were affected in vEDS, which suggests an abnormality in ER homeostasis, or stable equilibrium.
The ER, or endoplasmic reticulum, is an organelle inside cells that plays a role in the proper folding of proteins. An imbalance in ER homeostasis could affect the proper folding of the COLLIII protein and its function.
Lastly, researchers discovered that the levels of a collagen modifying enzyme called FKBP22 were significantly reduced, indicating another option through which the COLLIII protein structure may be affected.
“Our findings add new insights into the pathophysiology of this severe vascular disorder, since they provide a picture of the gene expression changes in vEDS skin fibroblasts,” the researchers wrote.
According to the team, mutations in COL3A1 can affect the structure and deposition of several structural proteins in the ECM, which is crucial to the integrity of soft connective tissues.
“Further studies are needed to delineate in detail the functional role of the identified gene expression changes in vEDS fibroblasts and to identify distinct molecular signature(s) that may contribute to the mechanistic events that cause vascular wall weakness of this severe connective tissue disorder,” researchers wrote.