Immune Dysfunction Common in Hypermobile EDS, Study Finds
Immune dysfunction — including abnormal activation of mast cells and antibody deficiency — is common among people with hypermobile Ehlers–Danlos syndrome (hEDS) and those with hypermobile spectrum disorder (HSD), according to a U.S. study.
These findings suggest that hEDS and its associated tissue fragility may increase the susceptibility to immune problems, such as the abnormal activation of mast cells, tissue-resident immune cells that are activated by tissue damage and drive allergic reactions.
Further studies are needed to confirm these findings and better understand the links between these conditions, the researchers noted.
The study, “Mast cell activation disease and immunoglobulin deficiency in patients with hypermobile Ehlers-Danlos syndrome/hypermobility spectrum disorder,” was published in the American Journal of Medical Genetics’ Seminars in Medical Genetics.
Hypermobile EDS, the most common type of EDS, is characterized by soft, smooth, and fragile skin, hypermobile joints, frequent joint dislocations, and inflammation. People with joint hypermobility who do not fulfill the criteria for hEDS are diagnosed with HSD.
Several previous studies reported a link between hEDS/HSD and mast cell activation disease (MCAD) and low levels of antibodies, or immunoglobulins (Igs).
Besides promoting allergic reactions, mast cells also help counteract the damaging effects of venoms and parasites. They are activated by specific molecules released upon tissue injury or inflammatory pathways.
MCAD is characterized by allergic symptoms such as asthma, hives, swelling, heart rate changes, and gastrointestinal problems. These can occur individually or all at the same time as a multisystem response.
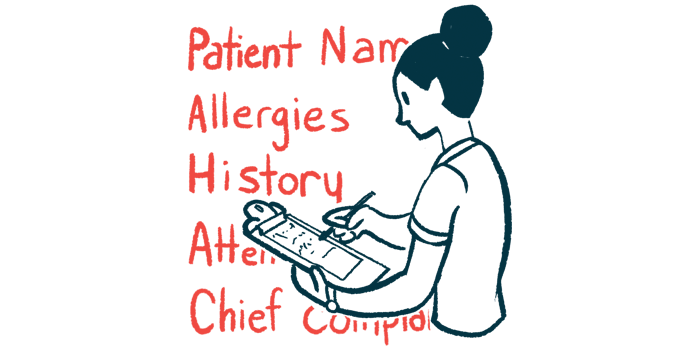
Given the potential link between these often underrecognized and undertreated conditions, a team of researchers in the U.S. analyzed their simultaneous occurrence among 974 patients with suspected MCAD.
Nearly three-quarters (74%) of patients were female, and all had been referred to a community-based allergy/immunology clinic in Tarrytown, New York, between 2015 and 2019.
The team retrospectively analyzed the patients’ electronic health records for diagnostic codes for MCADs, Ig deficiency, and hEDS/HSD.
Results showed that 496 (51%) of cases had a combination of at least two of the three conditions.
Specifically, MCAD and Ig deficiency were simultaneously present in 207 (21%) patients, while hEDS/HSD was combined with MCAD in 101 (10%) and with Ig deficiency in seven (0.7%). A total of 181 (19%) patients had a combination of all three syndromes.
This meant that 289 (29.7%) patients were diagnosed with a combination of hEDS/HSD and either MCAD or Ig deficiency, or both. Nearly half (45%) of all Ig deficiency cases had hEDS/HSD, which was the exclusive diagnosis of seven (0.7%) patients.
The simultaneous occurrence of hEDS/HSD and MCAD, as well as of all three conditions, was about four times higher among females than in males.
This is consistent with findings from previous studies, and these sex differences may be explained with “the presence and impact of hormone receptors on the activities of the epithelial layer and mast cells,” the researchers wrote.
“Further studies into the hormonal influences within these comorbidities [simultaneous conditions] are warranted,” they added.
While this study was based on patients suspected for MCAD, it highlighted “the presence of immune dysfunction in patients with hEDS/HSD, either MCAD, PID (Ig Def) or both,” the team wrote.
Given the role of mast cells in tissue defense and repair, “the overlap of MCAD and hEDS/HSD associated disorders likely reflects altered interactions between this innate immune cell population and the surrounding microenvironment,” the researchers added.
“This study implicates the susceptibility to tissue damage via the underlying tissue fragility which defines hEDS/HSD,” the team wrote.
Based on these findings, “we recommend screening for both MCAD and [Ig deficiency] as part of the evaluation of hEDS/HSD and the initial screening of all MCAD patients for hEDS/HSD,” they added.
Future research is needed to identify “underlying contributors to recurrent/chronic inflammation and tissue injury,” which may not only add insights on the underlying mechanisms of hEDS/HSD, but also help “tailor and personalize therapies” for these patients, the researchers concluded.