Spinal fusion carries greater risk of complications for EDS patients
6 times higher risk of degeneration of unfused bones next to fusion site: Study
Written by |
Following surgery to fuse the vertebrae in the lower spine, people with Ehlers-Danlos syndrome (EDS) have a six times higher risk of degeneration of the unfused bones next to the fusion site, a study suggests.
However, this complication, called adjacent segment disease (ASD), was not associated with the success of the surgery or with new cases of medical and surgical complications due to any cause, data show.
“These results suggest that EDS may predispose patients to longer-term postoperative complications such as adjacent segment disease,” researchers wrote.
The study, “Ehlers-Danlos Syndrome is Associated with Increased Rates of Adjacent Segment Disease Following TLIF: A Propensity Matched Study,” was published in the World Neurosurgery journal.
Hypermobile joints in EDS can lead to lower back pain, disability
EDS is a group of connective tissue disorders marked by unusually mobile joints and fragile, stretchy skin. Most known EDS-causing mutations affect collagen, a group of structural proteins that give bodily tissues their structure, strength, and shape.
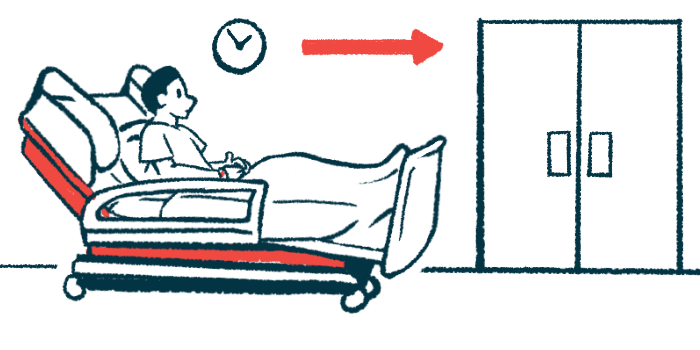
With such flexibility, EDS patients can experience excessive movement between the vertebrae in the lower spine (lumbar), which may lead to lower back pain, disability, and limited physical activity.
Transforaminal lumbar interbody fusion (TLIF) is a surgery that involves removing the spinal disc and fusing the bones for stability and pain relief. However, in some cases, degeneration of the unfused vertebrae adjacent to the fusion site, or ASD, can occur.
Despite having a known risk for surgery complications, whether people with EDS are at risk for ASD after fusion surgery is unknown, according to researchers at the University of Cincinnati College of Medicine, in Ohio.
“The objective of this study is to compare the rates of ASD among patients with EDS and those without EDS,” the team wrote.
Among those who underwent TLIF surgery between 2010 and 2022, 85 EDS patients were matched with 85 non-EDS patients based on equal numbers of medical and surgical factors that may contribute to ASD. The study’s primary outcome was the development of ASD within three years of surgery, as defined by the need for additional lumbar surgery.
The most common co-existing conditions among the patients, of whom 78.8% were women, were high blood fat levels (49.4%), high blood pressure (45.9%), depression (32.9%), and acid reflux (32.9%).
Adjacent segment disease much more prevalent in EDS patients
Data showed the rate of ASD was about six-fold higher in EDS patients compared with those without the disorder (52.9% vs. 9.4%). The risk of developing ASD within three years of surgery was 82% lower in patients without EDS.
“The significantly higher rates of ASD are hypothesized to be due to impaired collagen and its role in wound healing, blood clotting, and structure and elasticity of tissues,” the team noted.
The researchers found no difference in the occurrence of pseudoarthrosis, when spinal fusion fails, within two years of the surgery between patients with or without EDS. Likewise, no significant differences were found in the incidence of medical and surgical complications due to any cause within 30 days of the surgery.
“Those diagnosed with Ehlers-Danlos Syndrome have a higher risk of adjacent segment disease at 36 months after [TLIF surgery],” the researchers concluded. “The results of this study provide valuable insight for surgeons in consideration of TLIF procedures for patients with EDS.”







