vEDS diagnosed in man, 25, after ruptured aneurysm: Report
Rupture of blood vessel bulge occurred years after bowel perforation
Written by |
After experiencing a ruptured aneurysm in the hepatic artery — a blood vessel that supplies the liver — years after surgery for a perforated bowel, a 25-year-old man in Japan was diagnosed with vascular Ehlers-Danlos syndrome (vEDS).
According to the report detailing his case, the man had been given no medications in the decade or more between the perforated bowel he experienced as an adolescent and the severe abdominal pain and rupture of the aneurysm — a bulge in the wall of a blood vessel — that led to this hospitalization. The man was found, after admission to the hospital, to also have several aneurysms in the celiac artery, a blood vessel whose branches supply the stomach, spleen, pancreas, and liver.
“Juvenile-onset [bowel] perforation and rupture of the celiac artery are important findings in the suspicion of vascular-type Ehlers-Danlos syndrome,” the researchers wrote.
The study, “Vascular type Ehlers-Danlos syndrome with intra-abdominal hemorrhage due to ruptured hepatic aneurysm: A case report,” was published in the journal Acute Medicine & Surgery.
Man’s vEDS diagnosis confirmed with genetic testing
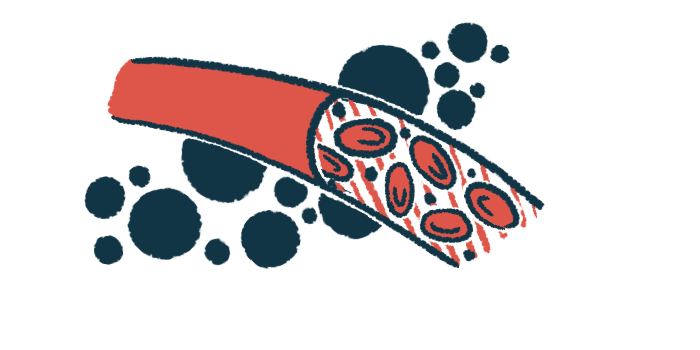
People with all EDS types typically have joint hypermobility, in which the joints move in a wider range than normal, and unusually fragile and stretchy skin. Individuals with vEDS also have fragile arteries and internal organs, which are more prone to bulging or rupturing. As such, vEDs is associated with a high mortality rate due to the risk of severe bleeding.
Here, a team of researchers from Wakayama Medical University described the case of a man with several aneurysms in the celiac artery and a rupture in a hepatic artery aneurysm. The patient had a history of perforation in a part of the large intestine called the sigmoid colon, which had required laparotomy surgery 12 years prior.
The man was admitted to the hospital with acute abdominal pain, which was repeatedly relieved but then worsened after taking painkillers. On day nine in the hospital, he experienced hemorrhagic shock, a condition characterized by a reduced supply of oxygen and nutrients to tissues due to severe bleeding.
The patient was transferred to an emergency medical center, where further evaluation found he had a fast heartbeat and fast respiratory rate. He also had pain or discomfort in the abdomen.
A CT scan revealed the presence of aneurysms in the celiac artery, rupture of a hepatic artery aneurysm, and bleeding in the abdomen. The bleeding required massive blood transfusion and a procedure caused angioembolization to block the blood supply to target tissues.
After the intervention, the man had a temporary increase in the blood levels of alanine transaminase — an enzyme that serves as a biomarker of liver damage. Levels of C-reactive protein, a marker of inflammation, were slightly high by day 12. Twenty days after he was admitted, the patient was able to walk and was discharged on day 26, after rehabilitation.
Our patient had been under no medication for over 10 years since laparotomy for colon perforation. Earlier prescriptions may have prevented the progression of the aneurysm.
The man had several clinical signs of vEDS, including stretchy and translucent skin, hypermobile joints, and a small jaw. Further analysis revealed the presence of an aneurysm in the carotid artery, which supplies the head.
The vEDS diagnosis was confirmed in a genetic test that revealed a COL3A1 gene mutation. The patient started treatment with celiprolol, an experimental therapy for vEDS that aims to reduce pressure in blood vessels prone to rupture. Celiprolol is used to treat high blood pressure.
At the last follow-up, the patients’ aneurysms remained stable.
“Our patient had been under no medication for over 10 years since laparotomy for colon perforation. Earlier prescriptions may have prevented the progression of the aneurysms,” the researchers wrote.