Surgery successfully repairs aneurysms in vEDS: Case series
Example shows instances when open AAA repair is 'feasible,' researchers said
Written by |
Nonemergency open surgery can safely and successfully repair abdominal aortic aneurysms (AAAs) in people with vascular Ehlers-Danlos syndrome (vEDS), according to a study of three cases.
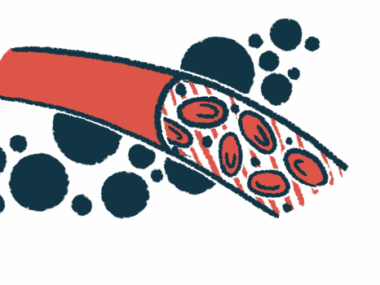
AAAs are bulges in the aorta, the large artery that runs from the heart to the abdomen. Because vEDS is associated with weakened blood vessels, an AAA is usually repaired only after it ruptures.
In these cases, surgeons used special techniques to ensure the integrity of fragile tissues while performing the repairs and prevent potential life-threatening bleeds and emergency care. Details of the procedures were published in the Journal of Vascular Surgery Cases, Innovations and Techniques in “Open repair of abdominal aortic aneurysms in patients with vascular Ehlers-Danlos syndrome.”
vEDS is a type of EDS, a group of genetic diseases marked by defects in the connective tissue that holds the joints and tissue together. As with other EDS types, a feature of vEDS is fragile skin that bruises easily. It’s also associated with a higher risk of blood vessel aneurysms, ruptures, and life-threatening bleeding.
AAAs are estimated to occur in up to 29% of vEDS patients. While surgery is an option to repair them, blood vessel weakness and the risk of uncontrolled bleeding have been associated with worse surgical outcomes. As a result, some surgeons avoid elective (nonemergency) repair surgery and operate only after life-threatening hemorrhages occur.
However, “elective surgery is anticipated to have superior outcomes than waiting” for a rupture to happen,” the researchers wrote, noting “contemporary data have demonstrated AAA repair can be performed safely” in vEDS patients.
When elective surgery for abdominal aortic aneurysms is ‘feasible’
Researchers at the University of Washington and the University of Rochester detailed the elective surgical repair of AAA in three vEDS patients, and described their techniques and patient outcomes.
All three, two women (ages 38 and 64) and one man (age 45), showed bulging of the aorta on CT scans. Each carried a different mutation in their COL3A1 gene, the underlying cause of most vEDS cases.
AAA open repair surgery involves sewing a manmade piece of artery into the aneurysm region of the aorta.
Before surgery, the patients were given medication to control their blood pressure to prevent the increase that occurs when the aorta is clamped to stop blood flow during repairs.
Extra blood products were made available to anticipate the need for transfusions, which occurs in 38% of open AAA surgeries in the general population, the researchers noted.
The patients’ chests were opened with gentle pressure using padded retraction blades to help avoid manipulating tissue too much. A unique soft fluid drain was used to distribute the force over a broader surface area and provide padding at the site of the aortic clamp.
After aortic cross-clamping, the aneurysm sac was opened and adjacent arterial sections were sown together with gentle knots to avoid tearing. The ends of the aortas were wrapped in felt to reinforce the arterial walls.
Extra precautions were taken with the 38-year-old woman with a COL3A1 mutation associated with a more severe vEDS. The researchers observed that her aorta was the most fragile. A patient with a less severe mutation had more robust blood vessels.
“This finding is consistent with the natural history of VEDS in which clear variations exist in the [presentation] and survival according to the underlying variant type,” the researchers wrote. “Understanding the type of COL3A1 variant can help with preoperative surgical planning and anticipating the quality of the tissue to be encountered.”
After surgery, the patients were transferred to the intensive care unit, where normal blood pressure was actively maintained. Over a follow-up that ranged from seven to 26 months (more than two years), none of the patients had complications or arterial aneurysms.
“Open AAA repair for patients with VEDS is feasible in the setting of a known diagnosis, knowledge of the COL3A1 variant, modification of the surgical technique to support the lack of aortic and arterial tissue tensile strength, and use of multidisciplinary perioperative team approach,” the researchers wrote. Perioperative refers to the time immediately before, during, and immediately after surgery.
“These cases demonstrate a genotype-surgical [presentation] correlation in vEDS and add to our growing understanding of surgical repair options for this population,” they said.